
At 1:02 am on December 10, 2022, two days after posting this blog, Joyce Stuber went home to glory. Right now she is kicking up gold dust in heaven in what is probably her greatest time. Whole. For the first time in her eternal life not suffering any physical or mental limitations. Free. REALLY free. I may be sad but cannot be unhappy for her. The day she went to the alter in 1992 and dragged Lorna and Leona with her, she started an avalanche that would transform not just one, but two, maybe three generations of our family for eternity.
Joyce’s story
It is probably time I write this story. I haven’t posted any blog in some time. I have been distracted by a medical crisis that my wife has been suffering through, pretty much all year. Even as I write this my wife is trying to recover from two emergency left side brain operations. 24 hours and only no purposeful movement or response. But then her head is still swelled from traumatic surgery. I am patiently waiting.
If anyone can survive brain surgery it is Joyce. May 6, 2003 Joyce had a brain tumor removed from her right temple. Spent two weeks in a coma and bounced back better than ever. I have seen so many miracles with this woman I don’t have enough fingers and toes (or even body parts) to list them all. I am also mindful that I must temper what I write so if she suddenly regains awareness and reads what I have written , if it is embarrassing or too personal she will kick my butt and give me and the world an earful. If there is anything YOU can do it is pray. Join an army of prayer warriors.
How this all started
Joyce had been coughing all winter, living on cough drops. Her primary doctor sent her to a Pulmonologist Morgan Meeks who could find nothing. Except. She had unusually high eosinophils. Those are specialized white blood cells that go after allergens. She tested her for every allergy and could find nothing. Meantime, a heart doctor was consulted. Dr. Mitchel Rashid did a heart cath and said she was pretty good except the finest blood vessels around her heart where veins met arteries (capillaries) were partly blocked so he put her on a mild nitrate to unblock them. A few months later on May 5th they called her into his office for an echo with Doppler. She told me as we were leaving that they literally called every tech, nurse and person in to see it since “they had only seen this in text books.” When she asked what was going on she was told: “Liability. We can’t say. But your doctor will call you when he sees this.” (Note: He never did call). We left his South Charleston office directly to our youngest daughter, Leona’s house in Beckley. That was May 5th. Joyce was to stay at her house feed dogs and cats while their whole family left for Virginia Beach. That was a Friday and I was to return to Clay County and work Monday thru Wednesday and then join her. She had breathing problems and was so weak she was mostly bed ridden that weekend, and the entire week, really. I stayed the week to feed animals. She refused to see doctor using her nebulizer when it was hard for her to breathe. I told her I would just wait till she passed out and call an ambulance. Leona was due back Saturday but I finally talked her into going to Med Express a few miles from Leona’s house on Friday the 13th. Andrew had arrived home early as we were headed out. I got her there and asked for help getting her in. She needed a wheel chair. She never made it in the door. As I was filling out paperwork, they checked her oxygen which was 22% and called an ambulance. When it arrived I was asked this question: Raleigh General or Beckley Appalachia Regional Hospital? I asked which is closer to here? BAR-H. So we went. It was 5 miles from Leona’s house.
The BAR-H Experience
Friday the Thirteenth in the ER. Do I have to say more? There were eight guernies ahead of us in the hallway waiting to get admitted to ER. It was a five hour wait. Once we got in the ER they did a chest x-ray and put her on oxygen. Then another four hour wait. As a nurse came by I asked about the doctor and the x-ray. I had seen the x-ray as they took it. Many big white blotches all connected with what looked like spider-webs. Nurse said, “The doctor is on his way and has seen the x-ray. It looks like Covid.” My heart sank. Seemed like a death sentance for a woman who had refused the Covid vaccines and had survived Covid twice in 2021. Two hours later the doctor arrived. “We are admitting her,” he said. “Covid?” I asked. “No.” He said, “Double pneumonia. She is lucky to just be alive.” After 12 and a half hours after arriving at the ER, Joyce was admitted.

It was touch and go the next two days. On Monday, with Leona back, they decided to drain out fluid from under her lung. 600 ml under one lung. 400 under the other.

They also gave her a heart echo and advised us they found a blood clot in her heart. This was the anomoly they found in Rashid’s office. He had never called us. We asked the hospital to call him. They said they tried, wanting records. Maybe I could. I did. Ended up arguing with a ‘Kim’ about the urgency of having Rashid call us back. He never did. She spent 15 days at BAR-H recovering from Double Pneumonia mostly on steroids and anti-biotics.
They released her to Leona’s house five miles away. She was so weak from loss of muscle tone we had to lift her off the bed and help her walk to the bathroom. Yet she refused physical therapy coming to see her. She insisted she would do this on her own. We scheduled appointments a week from release with both Meeks and Rashid. We requested both get her BAR-H hospital records prior to us seeing them. Joyce was stepped down from antibiotics and steroids. That was a mistake as you will see. She was sent home on oxygen.
The interim doctor experiences
We saw Meeks first. She, we discovered, is only a PA working for what doctor we never knew. She still could not explain the super high eosinophils but wanted to do a ‘parasite’ blood test. We did the blood test. Next day we saw Rashid. Correction. We saw his PA Holly. Apparently Rashid was too busy to see a heart clot patient recently released from the hospital. They had neglected to request records so I gave a verbal account. She scheduled a ‘tele-med’ appointment with herself for a month away.
The CAMC Memorial Hospital experience
Exactly a week later Leona rushes her mother who can’t breathe back to the ER. But this time to CAMC Memorial in Charleston, Joyce’s hospital, where all six of her doctors, including her primary doctor all practice. In the ER they would lose her oxygen tank and it would be a week before I could recover it. She had double pneumonia again. In the ER where I met her doctors, one of them (staff called an odd duck) was a young doctor Moorehead. He said: “I know what this is. West Virginia doctors have never seen this. It’s very rare. Hypereosinophilic Syndrome.” He had checked Meeks parasite test which was negative. Rare indeed. Only 1 percent of 1 percent of the world ever get this. The eosinophils when they don’t find allergens can attack blood vessels (like capillaries around her heart) the lungs (like infecting tissue causing double pneumonia) and the heart (creating a blood clot in the heart). If it goes on to the gastric and stomach it is too late and you can die. Luckily it had not gotten to that stage. He had trouble convincing others but they consented to his suggested treatment: the ‘atomic bomb’ of steroids. 125 mg three times a day for five days. It did the job. Killed out all the eosinophils. But. She went scitzophrenic and paranoid. She would have lucid waking dreams of a war going on outside. She would see nurses attacked and killed in the hallways. She would see dogs and cats wandering about. It took six nurses to hold her down to knock her out so they could put her on a ventilator and keep her unconscious for the four remaining days on the steroid ‘bomb’.

She had three teams: three pulmonologists; three hematologists and three heart doctors and the only thing they could agree on is that she was doing better on steroids by killing out the eosinophils. Nine doctors could not agree that it was Hypereosinophilic Syndrome. I saw the clot now a second time. Heart doctors there put her on Eloquis a blood thinner to mitigate its growth. It was bigger and clinging to the side of the heart chamber. All nine agreed to this: transferring her to Ruby Memorial in Morgantown where they could confirm the rare illness with a heart biopsy. So after fifteen days they packed her up and sent her to Morgantown. During her first Charleston stay I slept on a long bench in the Surgical ICU waiting room. This would change.
The Ruby Memorial Hospital Experience
Ruby Memorial had asked for her to be transferred so when we got there and spent the first couple of days in Surgical ICU I asked the heart team when they would do the heart biopsy to confirm the Hypereosinophilic Syndrome. The lead heart doctor laughed, “Lord no. We know the diagnosis is correct. We have seen all the echos and the MRI. We have seen the steroids do the job. We don’t need a biopsy to confirm. But we are glad you are here with this very rare clot so we can use this to teach a whole lot of young doctors.” Again she had a team of three heart doctors, three blood doctors and three lung doctors. It is impossible to get nine people to fully agree on anything. They added a tenth doctor: Dr. Pepper. Seriously. He was an immunologist and his job to keep eosinophils out of her body by a combination of adjusting steroids down and adding a Nucala infusion. (Upon her release she would get this infusion on the sixteenth of every month up to the present time at Summersville.) Over the next seventeen days she would be seen by multiple ‘classes’ during rounds. I signed permission for them to use these images and data in future classrooms. The blood team wanted to rule out a rare cancer so they did a bone biopsy on her hip. The poor Asian doctor had to almost stand on her to penetrate the bone. No osteoporosis in this woman. Her bones are STRONG. No bone cancer. Meantime I had arranged to stay at the hospitality house at the hospital. My church picked up the small nightly Rosenbaum House fee for which I am grateful. No sleeping in the car this time. Doctors took Joyce off Eloquis and had her on a blood thinner Heparin but transitioned her over to Warfarin (cummoden) before release. They said it had ‘more successful data’ than Eloquis. They also gave us Lovenox injections to inject into her stomach twice a day. They released her back to Leona’s because it was five miles from an emergency hospital. Our home in Clay County was 65 miles from a hospital. She was in danger of bleeding with a fall. And she was weaker than ever now.

Life away from her own home
She insisted upon getting up on her own to go to the bathroom but we wouldn’t let her. She was too week. But in the middle of the night if we weren’t watching she did anyway. One night she got up and after using the bathroom fell and banged her head and ribs on the bath tub. The next day we took her to the ER to get checked. Bruised but fine. Her right eye looked awful. She fell a number of times after, but on soft carpet or furniture. She insisted on going home. She loved her grandkids but activity was too much for her. Besides she missed her dogs. But my greatest fear is that she would get cut and bleed out (she was on cummoden a strong blood thinner) or have a possible stroke if a piece of the clot broke off and migrated to lung, a limb or brain. And if so, we would be 65 miles from a hospital in a place where Clay County ambulances are undependable. The day our tallest son Greg died in April 2020, both Brandy his wife and I called the ambulance and it took them 90 minutes to come seven miles. I didn’t want Joyce to die waiting on an ambulance.
A test of fath: the REAL test.
Youngest daughter Leona had a serious conversation with me about faith. If you took mama home, do you think God would just kill her? Of course not. You do think He is sustaining her even now? Yes. Well, take mama home. If the worst happens He will allow her to survive it. So I took mama home. Our youngest son, Chris and wife Melanie were staying at our property (in a camper they had moved in) feeding our dogs, their dogs, mama’s cats, Guinea pigs, two goats and 13 chickens in our absence. They weren’t really responsible for keeping our place clean and tidy and with our dogs in charge of our bedroom it looked like dogs were in charge. So upon our arrival mama, weak and frail started cleaning the house. I was muscle and gofer, moving furniture so she could sweep out under. We did three rooms. By the third day I was exhausted. When Sunday came up I told her I hadn’t been to church since this began so I wanted to attend. I gave her breakfast turned on tv, and asked her to stay in bed till I got back.
The worst realized
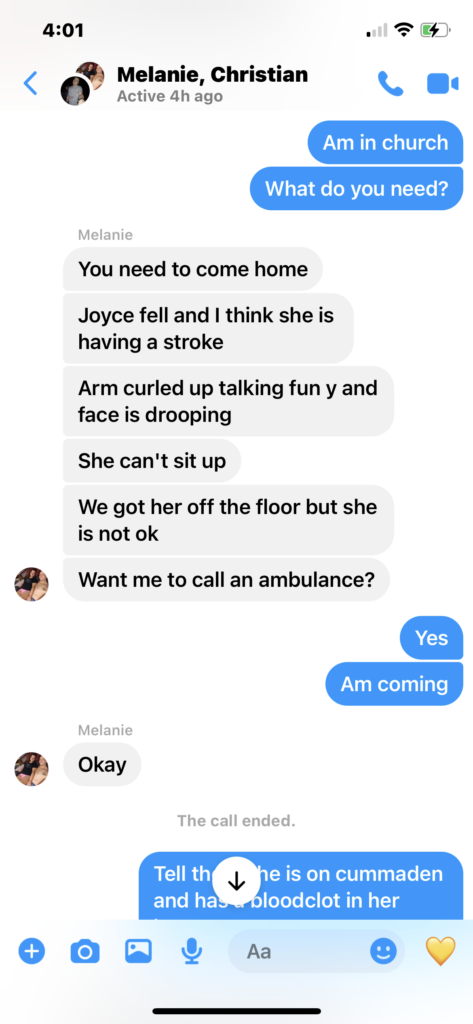
Little more than an hour later I got a text as the preaher began his sermon from my son Chris. “Joyce fell. Think she’s having a stroke. Arm curled and talking funny . . .” I left church immediately and drove home as fast as I could.
On the way I called Chris and asked him to call an ambulance. He said he tried and couldn’t get through. So I called. “I’m sorry.” The young male dispatcher said, “There are no ambulances in Clay County right now.” My worst fear was realized. “I can call one out of Kanawha County.” I said do it, I can meet them on I-79 at Clendenin. Once home Chris helped me lift her dead weight into the passenger seat and I flew as fast as possible through Elkhurst, through Clay, through Maysel and up Route 36 to I-79. I was approaching the Clendenin exit when I got a call back from the dispatcher. “Kanawha Ambulance is preparing to leave now. It will take them an hour.” I screamed back at him. An hour? I’m at Clendenin. I will be at the hospital in about 15 minutes. He said I will cancel the call just get her in. I did. My fastest time ever I arrived within the hour of placing the call to Clay Ambulance. I must have been doing more than ninety and I was hoping someone would stop me. I wanted an escort. When I pulled up to the door at CAMC Memorial ER a nurse who met me said “This woman is having a stroke. Where did you come from?” I said Clay County. She asked angrily: “Why didn’t you call an ambulance?” As much as I wanted to berate her, I let that go. Within 20 minutes without giving her anything (they couldn’t: she was on blood thinners) she started improving. She got some strength in her right leg. Her face improved a little and we could understand as she talked. Of course they admitted her and sent her upstairs. Back to Surgery ICU. However I learned quickly I could not sleep inside the building, let alone in the waiting room. A resurgence of Covid this spring had forced new policies for summer. At first I was sleeping in my car but one of the Social Workers found me accommodations at the local Hospitality House. My church again was willing to step up and help me, but the facility waived the fee, bless them.
A shocking image of old glory
I was aware that Dr. Lauren Searls was Joyce’s primary doctor at the Med clinic I always took her to see her at this hospital. But Searls is a resident. Joyce’s primary doctor (according to her insurance) is Dr. Andrea Stark. I met her for the first time at Joyce’s bedside as she took the helm of the team assigned to her. Joyce had a number of bleeds in her brain due to the stroke. They had to take her off blood thinners for five days while they waited for bleeding to stop. Those five days in July were intense as we were aware more strokes could happen. Basically they did nothing but wait. Well. That is not exactly true. She continued to show improvement from stroke damages. All but her right arm eventually. The third day there they sent in a young tech who had a portable Echo Imager with Doppler. As he looked at her heart, we watched the screen. What I saw was shocking. Images I saw before were of a big clot, but it always clung solidly to the wall of the upper left ventricular. Now, not only was it bigger, but it stuck out from the wall of her heart, and like a ‘ragged old-glory flag’ was waving in the chamber with every beat of her heart. The shredded stripes moving about on their own hanging tenuously as if they could break off at any moment. He was stunned and looked over at us. I told him, we knew about the clot since May. He was relieved. But this was NEW so we were stunned. It certainly explained the stroke. Some of the fringes had broken off and went to her brain. And could happen again. Actually it did, while she was hospitalized, and during a time when she was therapeutically on cummoden. After five days and the brain bleed had stopped, they first put her back on Heparin, and doing regular CT’s to see if brain was bleeding.
Shortly after she was on cummoden and at perfect range when she had a clot move to her thigh and cut off blood to her leg. They did emergency surgery to remove clot and save her leg. But we were at square one again. The only thing left to try was Pradaxa. They needed at least two doses in her before they could release her. Again with no guarantees she wouldn’t throw another clot somewhere. I remember the day well. I sat on the edge of Joyce’s hospital bed and Dr. Stark sat with me. She told me it would take six months to see the effectiveness of Pradaxa. I asked what are her odds of surviving six months. She said: “15 percent”. I said that is not good. She said, “You said you had an army of prayer warriors praying for her and it has worked so far. Count me in. I will be praying too.” She released us and we went back home.

Learning a new way of life
I was chief cook and bottle-washer, as well as butler, servant and perpetual company. And sometimes I had to do this while being berated. You see, Joyce had been manic depressive (bipolar) most of her life and managed well on Prozac. However the playbook went out the window after the stroke. She was mostly stuck in a manic (angry) phase. Occasionally this was a mixed phase as she would transition quickly to depression and remorse. It would take months to readjust her meds out of this and make her more even keeled. In the meantime she had a huge fall. And while I tried to get her seen upstairs for this by Dr. Searls, when she saw her she sent her downstairs to the ER there at Memorial. There she spent three days before being admitted and ‘watched.’ The bumps on her head were severe but ultimately did no damage. They did this out of an abundance of caution. Her fifth admittance was only five days in length there in September. She was sent home.
Finally hope restored
I had a one day surgery of my own having a spinal stimulator put in my spine, courtesy of the VA but surgery performed at Spine and Nerve center in Charleston. Finally I could do all this work mostly pain free. Later I would confirm with my own visit to the CAMC ER I had a hernia on my right side. I had first reported this to my VA doctor last spring. But he told me I did not. The VA Hospital arranged for CAMC Memorial physician Dr. Walker to see me on December 13. Joyce had an Echo with Doppler on October 20 that Holly at Rashid’s office had set up. So we went to CAMC Memorial Cardio Imaging and they did the echo. Eleven days later in Rashid’s office he himself told us the heart clot was gone. We were elated and told all the family the good news.
Why the setback?
But eight days later Joyce’s eyes went cross-eyed one morning. She couldn’t focus and it made her dizzy and nauseous. We took her to the local Primary Care but they urged us to go to Charleston and the emergency room.

We did. We were expecting an eye doctor. We got a whole trauma team. This was in fact another stroke. The eye righted itself but she was admitted where we discovered in a new Echo with Doppler that not only was the clot not gone, it was three times the original size. The November 8 event saved her life. We would have been ignorant of this till it killed her. She was they said, weeks away from a heart attack or congestive heart failure. Worse. Pradaxa the last miracle blood thinner failed her. Now, we were told that the same risky operation they were unwilling to do in August was her only chance of survival. Open heart surgery. She told doctor Kister yes. But a little more than an hour later another surgeon introduced himself, Dr. Alwair. He said he had a casual conversation about this surgery with Kister and had a different proposal: minimally invasive surgery going in from the side between ribs and he is right there at the top left ventricular. A small slice and can scoop the bulk of it out. Again she said yes. He said we need to get past three weeks ( November 29) from the stroke and would like to do surgery first week of December. To go past that was dangerous every day we delayed. But between the 14th and the twenty-ninth we had a Thanksgiving Day holiday. Suffice it to say (without assigning blame to names) people directly involved with applying to insurance and then scheduling surgery dropped the ball. No surgery was scheduled.
Straw that broke the camel’s back
The first weekend in December Joyce was both nauseous and had a massive headache. Monday December 5 it was all I could do to get her to the car by 9:00 am and grab my go bag and head to the CAMC Memorial ER. There again they said this was a stroke was largely unresponsive and transfered her to CAMC General to their Neurological Surgery department. She was immediately admitted. I slept in the car that night just outside in the parking building. Glad I did. I got the call at 2:16 am on Tuesday morning to come back inside.

I met a Nerosurgeon Dr. Orphanus who told me they needed to do emergency brain surgery on her left temple to take the pressure off her brain. He described everything I could expect in twenty minutes and I signed consent papers. Apparently it was not due to a stroke or fall but a weak blood vessel that burst. This aneurism is what caused the bleed and pressure. Likely her own blood thinners were the cause. We may never know. At 2:44 am they took her into surgery. It was the last time she would squeeze my hand after I squeezed hers. She was ventilated and could not speak. I waited in the waiting area. And he came out at 4:30 saying he did not leave a flap (a piece of bone out of the skull). He was hoping this would do. I got to spend 15 minutes with her before I had to go back to the car and sleep. At 11 when visitation resumed I was there. She looked worse. Swollen. And some of her wound was bleeding. I asked the nurse to ask her neurosurgeon if this was normal. They sent a Neuro PA who once she saw it called in Doctor Orphanus. He decided to take her first to CT than surgery where he did the operation again about twelve hours after the first. We had a long talk after about managing expectation for someone her age. Afterwards there was little response so I left her room early to sleep. I got there early on Wednesday December 7 and was told that new CT is good. Brain has expanded back. Worst source of blood was blocked. Neuro pathways are open and no pressure on the brain brain. He had left a flap this time and while she still looked swollen she should be getting conscious. Again how much she will gain back is the question. And, how soon. By the end of the day I got no response. No finger squeeze. Not a rise in blood pressure. Nothing. Only God knows if she is just taking a break or preparing to go home. Emotionally I am all over the map, but I am not hopeless. I have seen her turn around in situations as bad as this.
I am not in charge
Finally got a call from Dr. Alwair, her heart surgeon this morning. Says he has been following the case. Says heart surgery is off the table unless there is a miraculous recovery soon. He confessed he was dreading the surgery before because he imagined the surgery would have put her in the position she is in now. He does not expect her to recover. Her doctor say by Monday they have to remove ventilator and want to know if they can put a feeder in her stomach and an air vent in her throat. I will need to have an answer by Friday. But we had this prior discussion, Joyce and I: she did not want to live as a vegetable. We are following the Lord’s plan. I know this: he is doing what is best for her. As I write this December 8, 2022 there is still time. Still hope. And I wait. And I will see if she goes home with me, or home with Greg. We had discussed this many times, Joyce and I. Either way is a win-win for her. And that makes me smile.